Any condition or illness that affects a person’s urine is considered a kidney disease. Tumors, inflammation, and stone obstruction are all included, as are benign and malignant tumors.
Disease has an impact on bodily fluid maintenance, waste product release, and quantity. The interaction between these two functions can be used to explain a lot of kidney disease symptoms, and treating kidney disease symptoms in patients requires an understanding of this interaction.
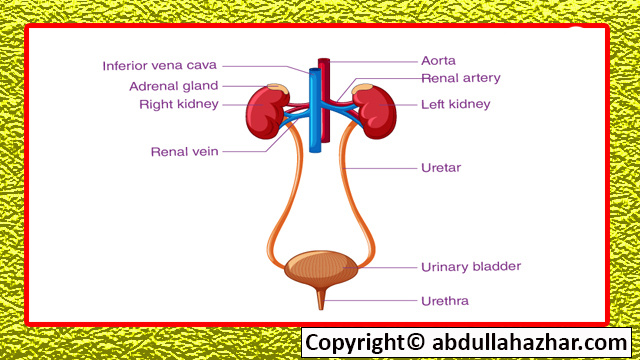
The process of excretion does not end with the production of urine; urine must pass through the ureters to the bladder, where it must be stored before being released, typically with voluntary control.
Changes in the urinary tract, infections, or diseases of the nervous system that cause the bladder to be dysfunctional can all have an impact on the entire process. Lower urinary tract obstruction is a significant source of discomfort and suffering, particularly in pregnant women and the elderly; it can result in serious kidney damage and worsen kidney function by obstructing urine output or allowing bacteria to enter the kidney.
Kidney Dysfunction’s effects on how the body works
A protein deficiency due to loss or an excess of water, sodium, potassium, or magnesium in the body are two effects of different types of kidney disease. Urine contains protein. Blood waste products from protein metabolism, such as urea and uric acid, as well as other nitrogenous compounds, like creatinine, can be brought on by kidney failure. There may be too much phosphate in the blood, which may cause low blood calcium for undetermined reasons.
Tetany, a condition marked by soreness and stiffness of the muscles, is brought on by a calcium deficiency, and as calcium is reabsorbed from the blood and other bodily fluids, calcium can also be lost from the bones. For illustration purposes, kidney-derived protein changes, alterations, and depletion have been treated separately; however, these diseases can and frequently are combined.
Features of Bodily Fluids
A crucial characteristic of body fluids is their total osmolarity or osmolarity because of how crucial osmotic forces are in determining how fluids are distributed within the body. It depends on the fluid’s concentration. While all solvents have an impact on osmolality, small particles like sodium ions or chloride ions actually account for more than 90% of blood osmolality because their effect is proportional to their weight.
The way the kidney produces water affects osmolality changes in kidney disease quite a bit. Water is lost from the body and causes a state of water depletion when the kidney is unable to store water or is not supported by the pituitary ADH to conserve water. Other times, especially when there are too many hormones present, the kidneys will retain too much water; renal system disease is the result of this hyperhydration, which can be treated by treating water intoxication and lowering the osmolarity of body fluids.
The acidity or alkalinity of body fluids is a crucial consideration. Renal system diseases like renal acidosis, which is caused by the kidney’s role in hydrogen ion release and storage, are characterized by the kidney’s inability to function properly.
A problem with the renal tubules, which one of their jobs is to convert weakly alkaline glomerular filtrate into (mostly) acidic urine, may be the cause of renal acidosis or it may be a symptom of kidney failure.
The composition of kidney products could alter, in addition to general changes in body fluids. The inability of many drugs to be excreted due to an increased concentration in body fluids is one of their problems. When viewed from the perspective of excretion, a rise in concentration will aid excretion and permit a sustained state of equilibrium at the rate of rise, but typically at a manageable concentration level.
For instance, a person with kidney failure should excrete the same amount of urea as a healthy person fed a normal diet, but they can only do so at a concentration of 100 mg of blood urea per 100 mL, not 25 mg. concentration.
Urea, creatinine, uric acid, phosphates, sulfates, urochrome, and all urinary substances that are simply “extracted” rather than “allowed” are substances whose concentrations are raised in this manner. Potassium must be mentioned because its storage is particularly risky and can result in cardiac arrhythmias. The use of artificial kidneys with semipermeable membranes and occasionally resins that absorb potassium in the intestines has made it possible to avoid this risk of kidney failure, which is now frequently avoided.
Disease of the Kidneys
Protein excretion in the urine is typically increased in various types of kidney disease, and urine frequently exhibits strong capillary clusters forming glomeruli permeability. In most cases, this elevated proteinuria—often mistakenly referred to as albuminuria—is 0.
daily intake of 5 grams or more.
Protein loss in the urine exceeds the liver’s capacity to make additional protein from available products when it exceeds 5 grams per day and stays at this level. The blood’s protein concentration declines, which leads to the formation of fluid in the blood. The body pressure in the capillaries usually releases fluid, whereas osmotic pressure is in equilibrium with plasma proteins, which have the function of retaining fluid, increasing the flow to the tissue sufficiently.
The lack of plasma proteins has an impact on how these fats are balanced. More water loss from the tissues leads to severe edema and renal system disease, both of which are made worse by the kidneys’ retention of salt and water. Nephrotic syndrome is characterized by edema, low blood protein levels, and high levels of protein in the urine.
This is a good illustration of the syndrome, which is defined as a well-known performance pattern with multiple potential outcomes. Nephrotic syndrome also includes chronic kidney disease and chronic kidney disease as examples.
Reduced Urine Flow
If there is little or no urine, the kidneys may not be producing any (oliguria), or the bladder or urine may be having an adverse effect on the kidneys. One kidney is present at birth in approximately 1 in 500 individuals, and kidney loss due to disease or accident is not unusual. As long as the other kidney is healthy, losing one kidney has no effect on a person’s capacity to eliminate waste.
The patient will experience an obstruction akin to the obstruction of the entire urinary tract in the event that the remaining ureter is completely blocked. The kidney failure section treats obstructive conditions, while the urinary tract disorders section treats partial or complete urinary incontinence.
Doug A. K. Black
Different urine flow patterns are affected when neural control is compromised, including (1) damage to the cerebral cortex or more from unconsciousness, which may result in different medical conditions. voiding inhibition Most of the time, psychological factors cause an ongoing urge to urinate, even when the bladder has a small capacity; urination is accelerated and continues until the bladder is empty.
(2) A side-to-side injury to the spinal cord above the sacral reflex zone or another injury (not involving internal organs) that first paralyzes the lower body before affecting the bladder. When the bladder is too full, the detrusor muscle relaxes and the urination reflex vanishes.
A small amount of urine is eventually released after the sphincter’s spasm is eventually overcome by increasing pressure. Overflow incontinence is the continued accumulation of partial and overflow urination. In these circumstances, the bladder can easily inflame, which can cause disability or even death from frequent urinary tract infections.
To prevent overstretching and induce an “automatic” period of the bladder, the bladder must be emptied using a catheter or by applying firm pressure to the abdominal wall. The internal sphincter relaxes more readily, the detrusor is not constrained by the upper part of the organ’s anatomy, which is small (about 150 ml), and the sacral portion of the spine controls it in harmony.
If the abdominal muscles are not paralyzed, they can assist voluntarily in this situation. Due to malfunction and the possibility of infection, there will, however, always be some leakage. Kidney damage can happen with the use of medication or, more frequently, if the pressure in the bladder does not decrease. This happens occasionally when the pressure on the bladder spreads to the kidneys.
(3) In contrast, damage to the central nervous system or the nerves supplying the bladder and urine below the Sacro chord reflex center causes bladder or “autonomic” problems. Even if the bladder were empty, there would still be 200–300 ml of urine present because the bladder is constricted but the contraction is weak. As opposed to automatic bladder overflow incontinence, this condition is referred to as active incontinence. Additionally, increasing the catheter’s urine output could be beneficial.
Kidney System illness
Dysuria, or painful urination, can be brought on by an infection of the lower urinary tract, though it is rare for chemicals to be the cause. Dysuria can be relieved by a good urination. additionally to mechanical stimuli brought on by tumors or stones.
Urinary frequency is frequently but not always related to dysuria. The actual amount of urine production may be abnormally high (polyuria), in which case urination will not be painful, or this may represent irritability or contraction of the bladder. Polyuria can occasionally only be detected at night (nocturia), when there is no polyuria during the day.
Kidney disease is indicated by severe pain and frequent urination; persistent polyuria is typically brought on by diabetes or kidney failure (difficulty swallowing). Nocturia is a physical condition that affects people who drink alcohol at night.
Defecation or urinary incontinence may result from nerve dysfunction that relaxes the sphincter muscles or from the bladder expanding too much. Patients in comas and those who have been injured, particularly the elderly, are frequently weak.
The sphincter that normally stops urine from leaking can be harmed by birth, benign prostatic hyperplasia, or other deformities of the bladder neck, in addition to blood vessel damage. It may be helpful to take bladder-stimulating medications. Additionally, more urine exiting the bladder via a different catheterization may restrict urine output.
When the nerve supply to the sphincter is compromised, programs have been developed to electrically stimulate the sphincter or schedule the bladder to empty on its own. However, the most effective products for severe pain are those that trap urine and stop contamination.
Ailments and Diseases of the kidney
This section draws attention to both kidney diseases and diseases that result in kidney failure for a variety of reasons. As a subset of the larger issue of urinary tract infections, kidney infections are treated later.
Too much renin produced by the kidneys can result in severe hypertension (high blood pressure) in chronic renal failure, and its effects can also affect the clinical picture. High blood pressure can harm the brain and retina in addition to other organs. Because high blood pressure affects the blood vessels in the kidneys, it can also harm them, starting a vicious cycle that is challenging to break. Due in part to the inability to produce erythropoietin, anemia is also frequently severe.
Infections and other issues, such as vomiting or diarrhea, can occur in patients with kidney failure, and they may require specialized care.
A low-protein diet (18–20 grams of high-quality protein per day) can help prevent kidney damage from occurring when symptoms of kidney failure start to appear. renal system disease Dialysis or a kidney transplant are the only treatments that can keep people alive when they are in the final stages of kidney failure.
Glomerulonephritis
Glomerulonephritis is a condition also known as Bright’s disease or nephritis. The disease mostly affects the glomerular clusters’ blood vessels. The suffix “-itis” designates an inflammatory condition, and glomerulonephritis is unmistakably linked to an infection given that it can develop soon after a streptococcal infection and, in its advanced stages, lead to a variety of illnesses.
According to the immune system, it appears to be an illness of the body. Proteins (antigens) respond; they create antigen-antibody complexes in glomerular groups or, in rare instances, renal system disease, insert themselves into the glomerular capillary wall.
In any case, the circulatory system is how the antibody or antigen-antibody complex, which is a mechanism frequently referred to as circulatory complex disease, gets to the kidney. The glomerulus’s response results in glomerular injury. Foreign protein and complex deposits interact with other protein elements in the blood (see subsequent article) and draw circulating white blood cells and platelets, which then release tissue-damaging proteases and other chemicals.
The idea of glomerulonephritis is based in part on comparisons with the kidney damage brought on by allergies in animals and in part on the finding that the protein of the allergen builds up in ill glomeruli.
There is plenty of room for different immune system pathogenic primary and secondary stimulating mechanisms in the general concept of immune system disease.
They attribute this to simple glomerular injury, which eventually results in the glomeruli themselves becoming antigenic, producing antibodies, and having (or not having) T lymphocytes. This variation is supported by both the variations in disease patterns observed in the affected people as well as the changes in glomerular tissue observed using the same techniques and electron microscopy.
A sore throat or (less frequently) a strep skin infection will typically be followed by glomerulonephritis for one to two weeks. Other pathogens, such as some viruses and protozoa, might be in charge, though.
Some unusual macromolecules that are chemicals can also do this.
The child has a swollen face, enlarged ankles, low urine output, and bleeding. Upon examination, it was found that there was tissue edema and that fluid flowed easily under light pressure; the blood pressure and blood urea levels were also slightly elevated or lowered. Although glomerulonephritis is a serious condition, the severity of the disease does not necessitate any special care beyond renal system disease elimination of the condition or discontinuation of the protein and fluid restriction was brought on by the drug. Nine out of ten individuals are totally impacted.
It has occasionally been noted that rare diseases have higher mortality rates.
But when the disease’s symptoms are severe, a small percentage of patients will pass away suddenly or months later. Another possibility is that the patient seems to have fully recovered, with all signs and symptoms going away, but in reality, the disease process for the renal system disease is still ongoing, causing nephron loss, which eventually results in kidney failure.
This process typically takes many years, and aside from protein in the urine and small red blood cells, the patient usually exhibits no overt signs of occult nephritis. There is no need to assume that a patient has kidney disease if there is protein in the urine (proteinuria) even though there are no symptoms because asymptomatic proteinuria has a variety of causes and can later manifest in asymptomatic young people. kidney disease in people.
In conclusion, glomerulonephritis can result in renal failure for a short period of time, nephrotic syndrome after years of asymptomatic proteinuria, or nephrotic syndrome after a period of severe proteinuria. Even in those who have never felt or can’t recall pain, all these things can happen. Many glomerulonephritis patients’ kidney biopsies display a variety of glomerular responses, such as hypercellularity, basement membrane thickening and damage, and varying degrees of progressive glomerular damage. Glomerular disease completely resolves in healthy individuals.
Leave a Reply